CaHRU study presented at Abu Dhabi medical education conference

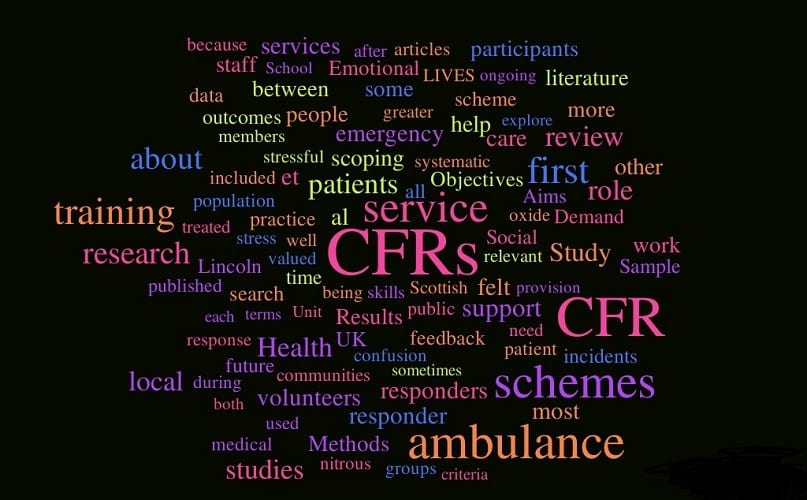
Dr Julie Pattinson presented at the Ottawa-International Conference on Medical Education (ICME), Abu Dhabi, United Arab Emirates; March 10th – 14th 2018. The conference is held biennially and provides a forum for medical and other health care profession educationalists to Continue reading CaHRU study presented at Abu Dhabi medical education conference